General information
reason
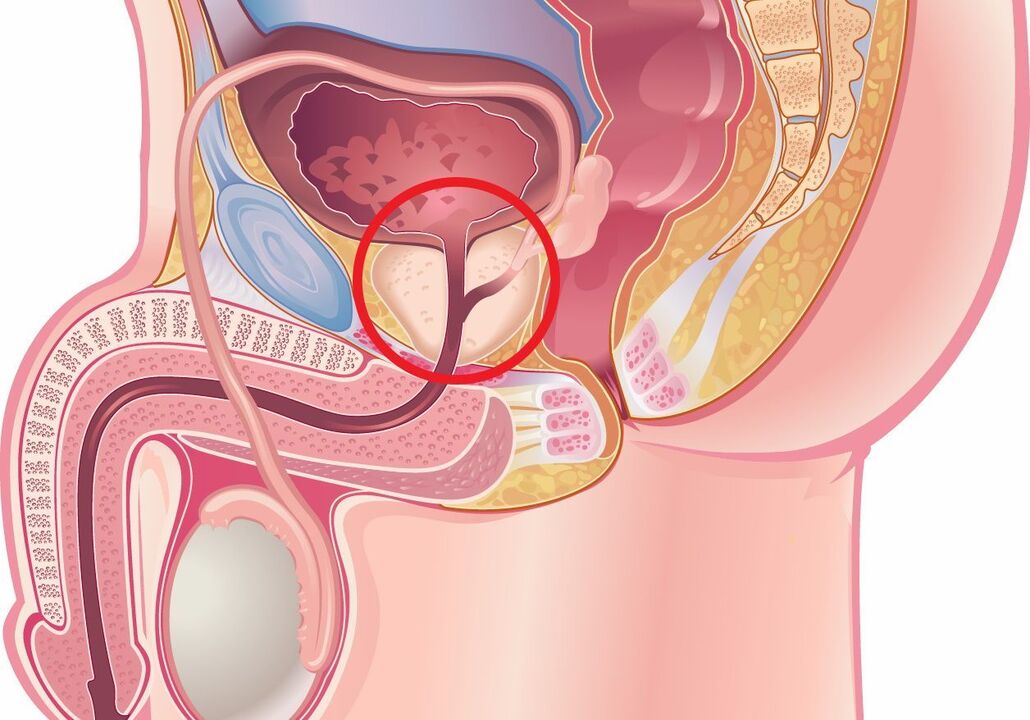
- Internal urinary system causes. Functional or structural pathology of the bladder: Cervical obstruction, inability of the external sphincter to relax during defecation, impaired detrusor contractility leading to urinary retention, and blood stasis due to vascular compression. Prostatic hyperplasia and tumors, urethral strictures, and obstructive bladder stones are also considered potential causes of venous congestion.
- compression. Circulation is impeded due to compression of the venous plexus by retroperitoneal tumors, metastases, and stool-filled intestinal loops (constipation). The blood vessels of the urogenital plexus dilate, blood flow slows down, the tissues are starved of oxygen and replaced by non-functional structures. Some of the blood settles and stops circulation.
- behavioral factors. Refusing sexual activity, irregular ejaculation, and using interruptions in intercourse as a means of preventing unwanted pregnancy can cause blood flow and prostate tissue swelling. During ejaculation, this gland is not completely emptied. Frequent masturbation can lead to congestive prostatitis because. . . For the development of an erection, blood flow to the genitals is necessary.
onset
Classification
- The first stage.It is characterized by the predominance of extravasation, exudation, arterial and venous hyperemic processes, leading to damage to the microvasculature and destruction of glandular tissue. These changes were recorded within the first few years after the onset of the disease. The clinical manifestations are most obvious in the first stage.
- second stage.An initial process of connective tissue proliferation begins to develop, and symptoms decrease. Due to thrombosis, microcirculation is compromised, thereby exacerbating sclerosis. At this stage, most patients experience sexual dysfunction: the intensity of erections and orgasms weakens, premature ejaculation occurs, and vice versa, men have difficulty reaching orgasm.
- The third phase. Severe fibrosclerotic changes are typical. It has been demonstrated that the proliferation of connective tissue is stimulated not only by inflammation but also by the ischemia accompanying congestive prostatitis. Complaints of dysuria are typical, and renal involvement in the pathological process is noted.
Symptoms of congestive prostatitis
complication
diagnosis
- lab testing. Microscopic and cultural examination of prostatic fluid is performed. Nonbacterial congestive inflammation was confirmed by a mild microscopic increase in leukocyte count and negative bacterial culture results. A PCR test is performed to rule out the sexually transmitted nature of the disease. In the third urine after massage, more pronounced leukocyturia was detected. To exclude bladder tumors, urine cytology can be performed; in patients over 40-45 years of age, a PSA blood test is reasonable.
- visual research methods. The main instrumental diagnostic method remains TRUS (bladder ultrasonography). The results of cystourethrography are important in confirming bladder neck dysfunction, revealing intraprostatic and ejaculatory urinary reflux, and urethral stricture. If the jet is significantly reduced, perform uroflowmetry. Assess pelvic floor muscle tone using a videourodynamic study.




































